Article at a glance
- Minority stress is a complex issue that affects the individual at hand but also stems to others in their inner circle and community as well. To learn more about minority stress and what it means, read this section.
Living with chronic stress can take a grave toll on one’s physical health and mental wellbeing. To learn more about the ways stress increases the likelihood of developing certain diseases and exacerbates chronic conditions, read this section.
Learning how to cope with chronic stress can be a long, multi-faceted process. To uncover the steps one needs to take to manage stress and different techniques on how to curb stress, read this section.
- When stress begins to affect one’s physical and mental wellbeing at a consistent rate, it’s important to reach out and ask for help from a physician. Mental health care comes in many different forms (individual vs. communal, online vs. in-person, etc.), so to learn more about the resources available, read this section.
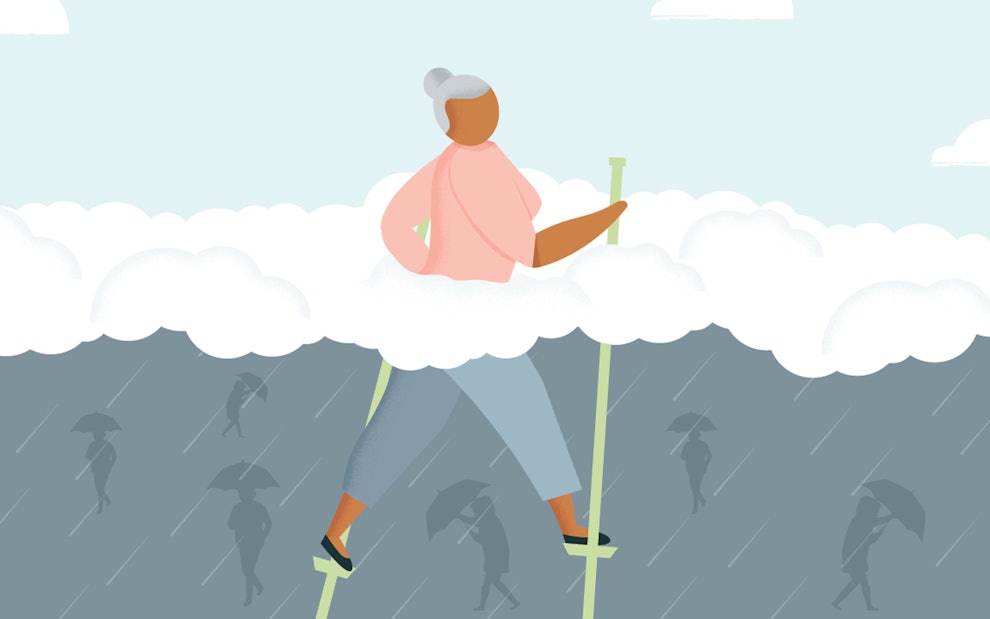
Minority stress refers to the additional stress the marginalized groups, including racial and sexual minority groups, have to face daily due to the prejudice, discrimination, and/or racism they face. This term surfaced in 2003 when the impacts of stress on marginalized LGBTQ+ groups were researched. Over the years, it has been explored further amongst all minority groups with studies proving that the impacts of minority stress on an individual can lead to an increased risk of developing a wide range of health issues.
Understanding Minority Stress
When evaluating stressors, it’s important to note that there are two different kinds: the active events a minority may face daily (physical violence, verbal discrimination, etc.) and the internal, emotional stressors that one may encounter regularly (internalized prejudice, feelings of rejection, etc.). Overall, these stressors may look like: financial issues, exposure to a high rate of violence, racial aggression, access to medical care, low comfort in medical settings, etc. It’s important to note that racism is an aspect deeply rooted in one’s society and thus, affects each institution embedded in that society. Due to this, minorities have likely faced discrimination through a variety of areas in their life that induce these stressors, including but not limited to housing, job security, food security, relationships, etc.
Through a study conducted by the National Institute of Health (NIH), 61% of American adults reported that they experience routine discrimination. When broken down further, 35% of African Americans, 35% of Native Americans, 25% of Latinos, 22% of Asians, and 18% of whites reported that they were unfairly not hired for a job. This information comes to show that, institutional racism, discrimination, and prejudice can affect one’s health through “both actual exposure and threat of exposure.” The study by NIH concluded by recognizing that in their findings, discrimination is linked to depression, anxiety, and various other psychiatric disorders. Furthermore, the study discussed that it’s common for these psychiatric disorders to live comorbidly in a patient, meaning that it’s common for a patient to live with more than one psychiatric condition at a time due to minority stress. Not to mention, it’s common for minority stress and its health effects to stem beyond the individual at hand and impact the lives of those close to them e.g. family members, caretakers, etc. If you are living with or providing care for a patient dealing with chronic stress, it’s important to be aware of the ways this stress may be impacting your life and health as well.
The Impacts of Stress on Health
Living with chronic stress is medically known to have a grave impact on one’s physical and mental health. When a patient is chronically stressed, in this case, a marginalized individual struggling with minority stress, their catecholamine, and suppressor T cell levels are raised, thus suppressing their immune system and greatening their risk of developing an illness. Some other medical findings of how stress affects the body include but are not limited to:
Releasing histamine and triggering broncho-constriction in asthmatic patients.
Altering insulin needs thus putting a patient at risk of diabetes.
Changing the acid concentration in one’s stomach increasing a patient’s likelihood of developing peptic ulcers, stress ulcers, or ulcerative colitis.
Increasing the plaque buildup in a patient’s arteries thus placing them at a higher risk of developing heart disease.
Generating risk for tumor growth in a patient along with the suppression of natural killer cells thus increasing their likelihood of getting cancer.
Living with stress each day is scientifically proven to exacerbate any chronic conditions a patient is handling in addition to increasing the probability of them falling into another illness. The main conditions triggered by stress include: cardiovascular diseases, asthma, high blood pressure, gastrointestinal disorders, and diabetes.
Ways to Manage Stress
Learning to manage stress comes in three steps: recognizing what’s instigating the stress in one’s life, curbing habits that dispose of stress in unhealthy ways, and then finally, attempting various stress management techniques.
Identifying the Root Stressors
When taking the steps to recognize what’s a stressor in your life, it’s important to scratch beneath the surface. For example, minority stress is the umbrella of what’s distressing a marginalized individual daily, but more specifically it’s their boss at work who actively discriminates against the patient. Be sure to fully evaluate and reflect on what is truly generating the stress in the various situations you confront daily.
Curbing Unhealthy Coping Mechanisms
After the various stressors have been identified, a patient can aim to cut back on unhealthy habits that are helping them cope with that stress. These unhealthy habits include but are not limited to: overeating, smoking, drinking in excess, doing various drugs, and oversleeping. While attempting to keep these habits in check, one should begin evaluating their stressors by the four A’s: alter, avoid, adapt, or accept. An example of evaluating a stressor in this fashion would be changing one’s environment to eliminate the stressor (alter) or developing coping behaviors to overcome the stressor (adapt). Relating to the example of a marginalized individual facing discrimination in the workplace, maybe a way to adapt is by submitting anonymous complaints to superiors about their boss or co-worker or perhaps finding a different job if that switch is feasible.
Implementing Healthy Stress Management Into One’s Daily Life
The last step in this process is having the patient uncover which stress management techniques work for them and help them maintain a healthy lifestyle physically and mentally. Common stress techniques include but are not limited to:
Various forms of exercise.
Connecting with loved ones.
Practicing relaxation techniques such as breathwork, working with essential oils, etc.
Working on time management throughout the day.
Maintaining a balanced, healthy lifestyle with food, sleep habits, and hygiene habits.
Journaling, reading, or discovering other forms of inspiration that incite one to keep a positive outlook.
Asking for professional help.
Learning how to manage stress is not an easy task and it may take some time before discovering which tactics work best for you. If stress is beginning to impede your livelihood and daily habits, such as inducing insomnia, long-term feelings of panic, fluctuations in eating habits, etc. it’s important to speak with a physician.
Note: To further visualize what a healthy and balanced lifestyle looks like, visit this source.
Stress and Mental Healthcare
According to the U.S. Department of Health and Human Service’s Office of Minority Health, racial and sexual minority groups are less likely to have access to mental health services and less likely to use community mental health services when offered despite their increased risk of having mental health issues. The need for mental healthcare can stem from the patient themself to their loved ones and their caretakers as well because minority stress is known to impact the communities of marginalized individuals. Furthermore, mental healthcare comes in all different forms to accommodate the various wants and needs of different patients e.g. individual vs. communal therapy, in-person vs. online therapy, etc. If you or a loved one is in need of mental health assistance, don’t be afraid to talk to a regular physician about how to get the help that works for you or contact one of the resources listed below.
The Effects of Stress on the Household
As a physician, we see a variety of patients greatly influence the lives of their families and caretakers. The impact they have is because it’s common for many minority groups to live commingled in a multigenerational household. However, the flip side of this influence, is that it’s also common for stress to spread from the individual to those they love and care for. The second-hand stress that caretakers and loved ones take on can be just as detrimental as the stress it originates from. This is why keeping an awareness of when one is stressed and where that stress is coming from, plays a key role in figuring out the best way to cope.
Considering COVID-19
In a study conducted by The Center for Public Integrity, it was found that 18% of Americans live in multi-generational households, putting older adults at a greater risk of getting infected. Part of the study stated, “These households often made up of people of color, who have less access to health insurance and higher rates of health problems that make COVID-19 deadlier.” This pandemic has been a tragic and stressful experience for everyone, but even more so for individuals living commingled with loved ones of all ages. The stress induced by COVID-19 for commingled, minority living situations links well to the overall image of what a stressor can look like for those affected by minority stress.
While there is often a social stigma related to therapy, there is well-established evidence that various types of therapy can improve mental health outcomes alone, or in conjunction with, traditional medications. Therapy can take on different forms such as traditional talk therapy, art therapy, music therapy, or pet therapy. Furthermore, these forms of therapy can occur with various types of mental health professionals, such as a psychologist, behavioral health specialist, and more. Outside of the medical field, many patients mentally benefit from activities such as meditation, yoga, and tai chi. When considering therapy, it’s important to understand all of the options made available to you so you can explore the ones that speak to your health needs and desires.
To learn more about the proper precautions to take during this pandemic while living in a multi-generational household, visit this source.
To discover where you can be COVID-19 vaccinated once you’re eligible, visit this source.
Mental Health Resources
Find a Therapist in Your Area
Call Centers
Substance Abuse and Mental Health Services Administration’s National Helpline: 1–800-662-HELP (4357)
Suicide Prevention Lifeline: 1–800-273‑8255 (TALK)
Suicide Prevention Lifeline for Hearing Impaired: 1–800-799‑4889
The Samaritans: (877) 870‑4673 (HOPE)
Trevor Project Lifeline – Hotline for LGBT youth, (866) 488‑7386
Child Help USA National Hotline – For youth who are suffering from child abuse, 1–800-4-A-CHILD (1–800-422‑4453)
Boys Town National Hotline – Serving all at-risk teens and children, (800) 448‑3000
National Teen Dating Violence Hotline – Concerns about dating relationships, 1–866-331‑9474 (or text “loveis” to 22522)
Text Hotlines
Crisis Text Line (Or, on your smartphone, text HOME to 741741)
Note: Oak Street Health has providers ready and willing to explain a patient’s medical insurance benefits to them. To learn more about mental health and how it’s covered in your insurance plan, including Medicare and Medicaid, visit this source.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3796016/
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246827
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6532404/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3341916/
- https://www.helpguide.org/harvard/stress-and-your-health.htm
- https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress-symptoms/art-20050987
- https://medlineplus.gov/ency/article/001942.htm
- https://www.helpguide.org/articles/stress/stress-management.htm
- https://www.minorityhealth.hhs.gov/omh/content.aspx?ID=9447
- https://www.heart.org/en/healthy-living/healthy-living-infographics
- https://www.oakstreethealth.com/what-is-behavioral-health-446277
- https://vaccinefinder.org/search/
- https://www.nbcnews.com/news/latino/latino-multigenerational-households-risk-covid-states-address-vaccine-rcna511
Become a patient
Experience the Oak Street Health difference, and see what it’s like to be treated by a care team who are experts at caring for older adults.



