Article at a glance
With the rapid production and rollout of the coronavirus vaccine, a lot of questions hang that patients want answers to. To learn more about general vaccine questions, such as which vaccines are available and when you can receive them, read this section
As with most vaccines, side effects are common as they indicate that a body’s immune system is properly responding. To learn more about the side effects associated with the COVID-19 vaccine and how to relieve them, read this section.
Many wonder about the vaccine’s long-term effectiveness and pose many questions surrounding the vaccine’s safety. Through various trials, all approved COVID-19 vaccines have proved to have high efficacy and safety rates. However, research into the vaccines and their success is ongoing as the virus continues to develop. To learn more about the vaccine’s efficacy, read this section.

According to the Center for Disease Control and Prevention (CDC), the coronavirus disproportionately affects older adults due to their weakened immune systems and various comorbid conditions. The majority of hospitalizations are attributed to those 55 and older and nearly all who have died are at least over 50. Due to the serious effects and risks this virus poses to older communities, they have been made the priority on vaccine rollout lists throughout the country. With so many dead and dying in our country and the world, it’s imperative to seniors’ health that they are vaccinated. But first, it’s necessary that they understand the benefits and risks that come along with the COVID-19 vaccination process.
Read more about covid vaccines for older adults below to learn how covid vaccines impact those with a weakened immune system such as seniors.

COVID-19 Vaccine and Preventative Care
Preventive care covers any routine service whose goal is to prevent future illnesses, conditions, or diseases. Certain routine services include but are not limited to recommended vaccinations, screenings, and/or check-ups. Examples of preventive care could be:
A patient visiting their dermatologist once a year to screen for any cancerous moles or skin patches to avoid serious illness
Getting an annual flu vaccine to increase immune response
Patients over the age of 50 getting a colonoscopy to screen for any issues in their colon and avoid any severe illness that could develop from it being infected
Preventive care is a major goal for healthcare professionals because it allows them to help their patients stop any problems before they even begin.
Knowing the benefits of preventive medicine aids a patient in understanding why receiving vaccines such as the COVID-19 vaccine is so crucial. Getting vaccinated helps a patient remain protected from the virus in case they encounter it in the future. Especially for higher-risk patients like adults in certain age groups and those with immunocompromising conditions, this vaccine is crucial as these groups are more likely to develop severe coronavirus symptoms or complications. Not to mention, the sooner every individual can get the coronavirus vaccine, the sooner we as a society can build herd immunity and eventually, eradicate the virus for the better of our collective public health system.

Preventive Care Tips
Understanding preventive care and how to incorporate it into your annual health care plan can be tricky. Here are some tips to guide you while making a yearly care plan and how to incorporate the COVID-19 vaccine into that plan.
Research and Plan: Prior to seeing a doctor or receiving the vaccine, it’s important to research it on your own. Doing so allows you to gather your own questions, comments, or concerns you might have regarding the vaccine and your personal healthcare needs. Write down any questions you have or concerns regarding the vaccine and current medical conditions. Writing things down before you go can help you to remember your thoughts and make sure you leave feeling knowledgeable about your decision.
Talk to a Doctor: Prior to receiving the vaccine, address any concerns you have and ask questions that are lingering in your mind. Costs and medical benefits are important to include in this conversation as well. An advantage of Oak Street Health is that their healthcare workers are prepared and willing to walk any patient through their medical benefits so they understand what they’re eligible for.
Location: Meeting with your primary care physician to receive the shot will boost your comfortability because you are familiar with them and they are aware of your healthcare wants and needs. Not to mention, if transportation is an issue, Oak Street Health is able to provide their patients with free transport to and from their facilities, so receive the shot in a place that is familiar and inviting.
General Vaccine Questions
Which vaccines are available within the United States?
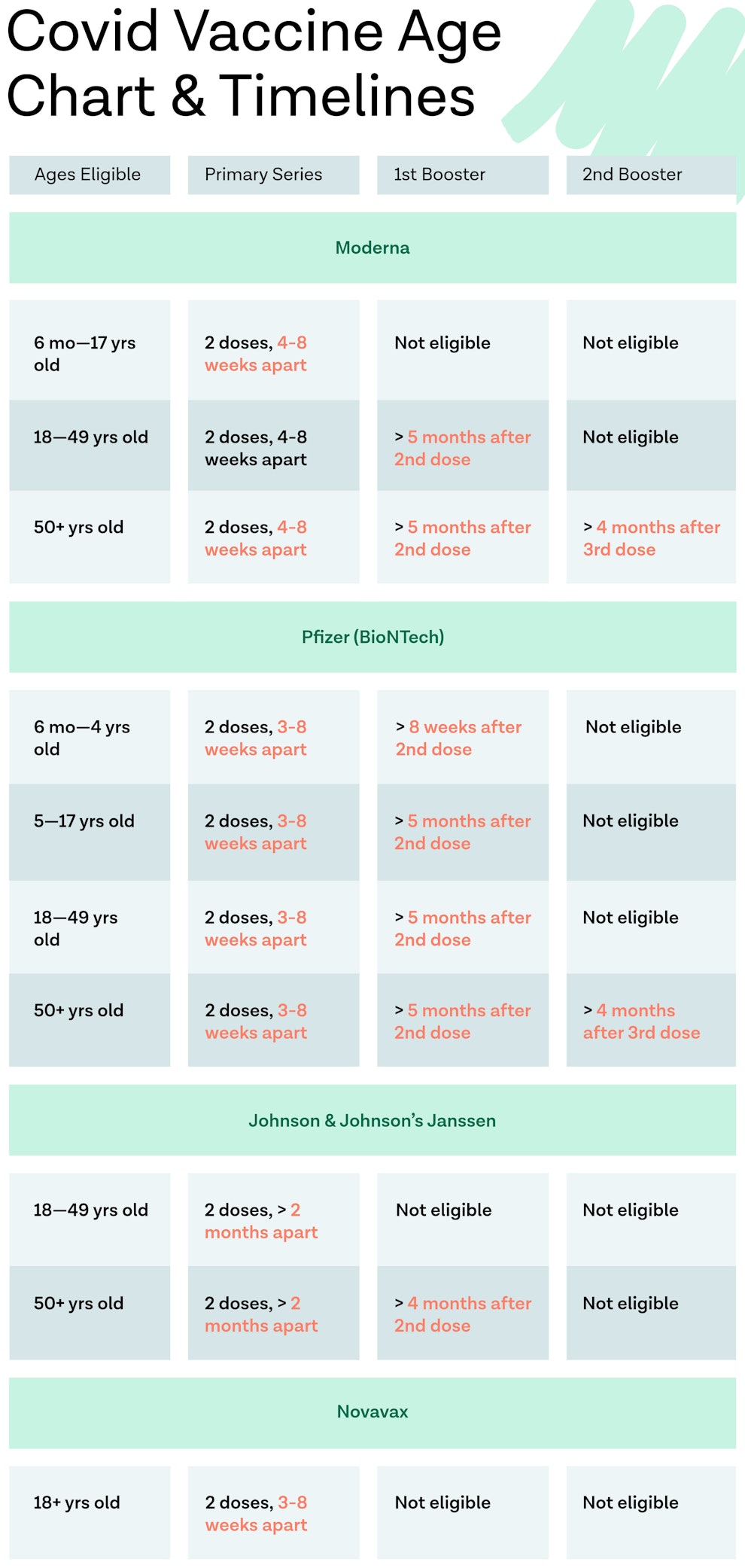
Currently, three vaccines are available within the United States which are the Pfizer vaccine, the Johnson & Johnson / Janssen vaccine, and the Moderna vaccine. Booster shots for each vaccine are also available at this time and it’s recommended to receive a booster dose from vaccine providers in the months after you become fully vaccinated.
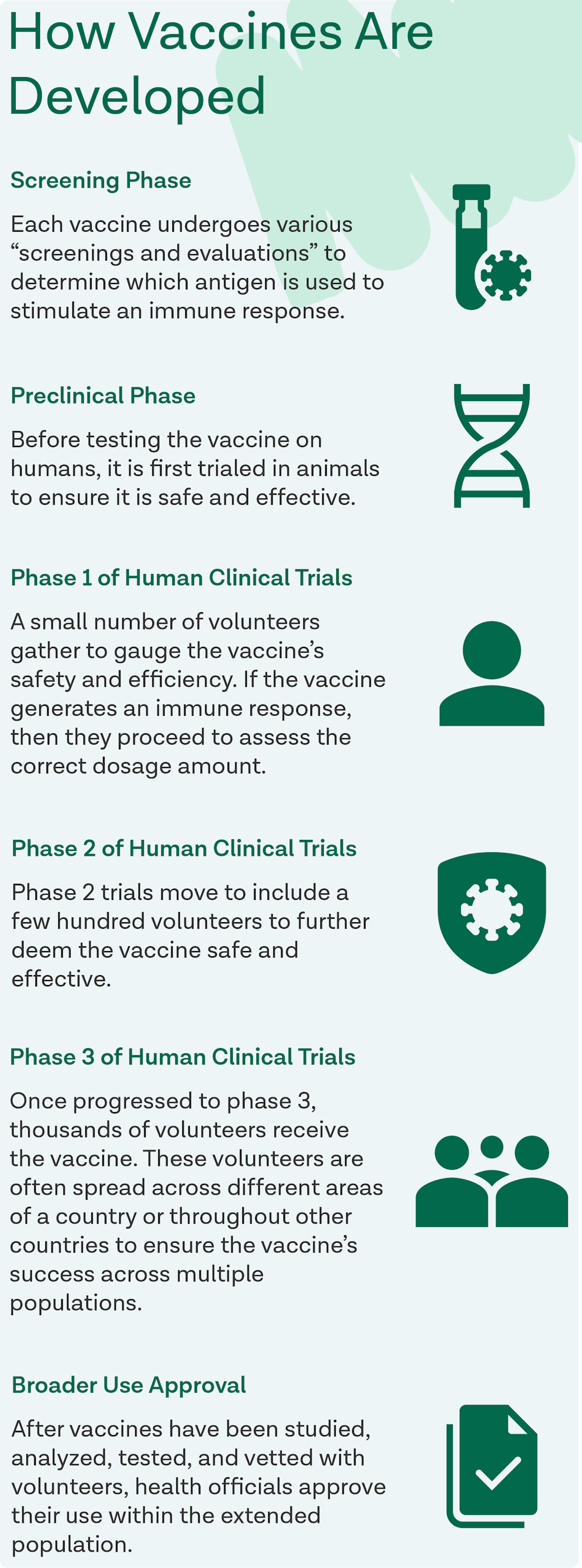
Vaccine development timelines were hastened due to the pandemic, leading all vaccines to be FDA-approved through emergency-use authorization. Now, the Pfizer and Moderna vaccines are fully-FDA approved vaccines.
Note: To learn more about the clinical trials vaccines went through and specifics on each vaccine, visit this source.
Does it matter which vaccine I get?
At this time, both the Pfizer and Moderna vaccines are proven to be highly effective and pose little to no safety concerns. Due to the Pfizer and Moderna vaccines being comparable, it does not matter which vaccine a patient receives, and is more important for the patient to get the first vaccine made available to them.
The Johnson & Johnson vaccine is proven to “plausibly cause” blood clots with low platelets (thrombosis with thrombocytopenia syndrome or TTS) in about 3.83 cases per million. These few cases have led to deaths. It’s encouraged to receive the Pfizer or Moderna vaccine over the Johnson & Johnson if possible.
Note: To learn more about the risks and potential adverse side effects of the Johnson & Johnson / Janssen vaccine, visit this source.
How does the vaccination process work?
Prior to getting vaccinated, it’s important to check your local health department regulations to ensure you are eligible to receive the vaccine or booster. All vaccines require multiple doses, meaning two doses of the vaccine and a subsequent booster dose.
Once it’s time to receive the vaccine, both the Pfizer and Moderna vaccines are administered in the patient’s upper arm. Before going home, the patient should receive a vaccine card or printout that lists the vaccine received, when they received it, and where they received it. For the Pfizer vaccine, the patient should return to get their second dose 21 days later. For the Moderna vaccine, the patient should return to get their second dose 28 days later. However, if a patient is unable to get their second dose appointment close to that timeframe, the CDC notes that there can be a maximum time of 6 weeks between the doses. The Johnson & Johnson vaccine is also administered in the patient’s upper arm, however it only requires a one-time dose upon first vaccination.
Booster shots are recommended for patients five months after their final dose in their primary vaccination series. Secondary booster shots are recommended four months after initial boosters. These shots are also distributed through the patient’s upper arm and are proven to lessen the side effects of COVID-19 if a patient gets infected.
It’s important to note that after receiving the vaccine, patients will be asked to wait 15 minutes before leaving the vaccine site to ensure they don’t have an allergic reaction or intense adverse side effects.
When can I receive the vaccine?
Oak Street Health is solely treating adults 65 and older who live near their facilities. However, there are other centers that offer vaccines to various groups of people.
The Center for Disease Control and Prevention (CDC) recommended that the first round of doses go to healthcare personnel and long-term care facility residents. From there, frontline essential workers such as firefighters, police officers, U.S. postal workers, etc., and those over 75 years of age should be vaccinated. From this point forward, those aged 65 and older, those over 16 years of age with underlying conditions, and other essential workers such as those in transportation, food service, etc., should be vaccinated.
Each state has the authority to design their own vaccination timeline and distribution plan which may affect booster shot rollouts. To learn more about the vaccine clinics provided by your local health departments in your state, visit this source.
If necessary, will Oak Street Health provide me with transportation to get the vaccine?
Yes, one of the benefits of Oak Street Health is that we provide free transportation to and from our offices if patients need assistance. Contact your local Oak Street Health provider today to learn more about this program.

Side Effect Questions
What are the side effects of the COVID-19 vaccine?
As with any vaccine, there are a variety of side effects that range from mild to severe depending on the patient and their immune system. With both the Pfizer and Moderna vaccines, it’s possible for side effects to occur after both doses. However, after the first dose, it’s more common to experience mild side effects at the injection site such as swelling, redness, and/or irritation. After the second dose, it’s common to experience full-body side effects that may include chills, low-grade fever, fatigue, and/or headaches. It’s important to note that these side effects should only last for a few days at most. Therefore, if feelings of discomfort endure, it’s important for a patient to contact their doctor. The Janssen vaccine has been linked to similar side effects (swelling around the injection site, fatigue, chills, low-grade fever, etc.) occurring after the first shot, but again these should subside within a couple of days.
Are those 55 and older likely to be more affected by side effects or experience adverse effects from the vaccine?
Many concerns were raised regarding the vaccine’s safety with older populations. However, studies show that older adults are actually less likely to experience side effects in comparison to younger generations. One study notes that the vaccine is “better tolerated in older adults than younger adults” and that its efficacy is similar across all age groups.
However, underlying conditions that are more common within older demographics (such as, heart disease, diabetes, kidney disease, etc.) can increase the risk of developing a severe case of COVID-19.
How do I diminish vaccine side effects?
Health officials recommend that patients should take acetaminophen such as Tylenol if a fever erupts and to heat or ice if their arm feels sore post-vaccination. However, it’s important to note that patients should not take these over-the-counter pain relievers (Tylenol, ibuprofen, Advil, etc.) before receiving the vaccine as they may weaken the vaccine’s efficacy.
How do I report adverse reactions?
After a patient speaks with their doctor and determines that they did or are experiencing adverse effects from the vaccine, they are encouraged to submit their story to the Vaccine Adverse Event Reporting System (VAERS). There is also a new system in place known as “V-safe,” which is a smartphone-based tool that sends patients surveys and check-in messages after being vaccinated. V-safe reminds patients to get their second COVID-19 vaccine dose, answers questions about the vaccine, and provides a place where patients can submit any concerns or side effects they experienced after being vaccinated.
Vaccine Efficacy Questions
If I already had COVID-19, do I need to be vaccinated?
Currently, it is unknown how long immunity lasts after a patient has been infected with COVID-19. Due to this, the Center for Disease Control and Prevention (CDC) recommends that even patients who have previously contracted COVID-19 should be vaccinated.
Patients with comorbid conditions such as COPD, heart failure, diabetes, chronic kidney disease, and obesity have been linked to a likelihood of hospital readmittance. Therefore, it’s especially vital for those with these conditions and those living in assisted living facilities to be vaccinated even after having the virus because they are the communities with the highest risk of readmittance.
If I am vaccinated, do I need to wear a mask and comply with social distancing?
Yes because even though a patient is vaccinated, there is a chance they are still able to asymptomatically spread COVID-19 to others.
Will booster shots be needed for the vaccine?
Yes, at this time booster shots are recommended for all available vaccines.
To learn more about booster shots and when to receive them, visit this source.
Can I get COVID-19 even if I’m vaccinated?
All vaccines have been proven to prevent severe illness as they are highly effective at preventing a patient from contracting the coronavirus. While it’s extremely rare, it is still possible that a patient may contract COVID-19 after being vaccinated. Full protection by both the Pfizer and Moderna vaccines does not commence until two weeks after the second dose of the vaccine. The Pfizer vaccine is proven to have 52% protection after the first dose and 95% protection after the second. The Moderna vaccine is proven to have 80.2% protection after the first dose and 94.1% protection after the second. The Johnson & Johnson vaccine is proven to have 66% efficacy after its one-time dose.
Vaccine Safety Questions
Can I receive other vaccines alongside the COVID-19 vaccine?
The CDC recommends that both vaccines are administered solo, without the interference of any other vaccines. A patient must not receive another vaccine within 14 days before or after getting their first or second dose of the COVID-19 vaccine.
Can I have the first dose be from Pfizer and the second be from Moderna i.e. can I mix vaccine doses?
It is recommended that a patient should receive the same vaccine for each of their doses. The vaccine type a patient received should be listed on the vaccine card given to them on the day they were vaccinated.
Vaccine Cost Questions
How much does it cost for me to get the COVID-19 vaccine?
Under the CARES Act of the federal government, the COVID-19 vaccine is free for any American that wants one. To learn more about COVID-19 vaccine coverage and costs, visit this source.
Note: One of the benefits of Oak Street Health is the support they offer in explaining which benefits patients are eligible for within their Medicare plan. While Medicare claims they cover the COVID-19 vaccine, COVID-19 tests, COVID-19 antibody tests, etc. on their website, an agent from our team would love to answer any and all additional questions you may have.
Sources
- https://www.medicare.gov/coverage/coronavirus-disease-2019-covid-19-vaccine
- https://www.oakstreethealth.com/
- https://www.goodrx.com/covid-19/how-much-will-the-coronavirus-covid-19-vaccine-cost
- https://www.kff.org/global-health-policy/issue-brief/the-coronavirus-aid-relief-and-economic-security-act-summary-of-key-health-provisions/
- https://www.aarp.org/health/drugs-supplements/info-2021/pain-relievers-covid-vaccine.html
- https://health.mountsinai.org/blog/what-older-adults-need-to-know-about-covid-19-vaccines/
- https://www.cdc.gov/coronavirus/2019-ncov/vaccines/expect.html
- https://www.oakstreethealth.com/covid-19-vaccine
- https://www.sciencemag.org/news/2021/01/new-coronavirus-variants-could-cause-more-reinfections-require-updated-vaccines
- https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
- https://vaers.hhs.gov/
- https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/v‑safe/index.html
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32481–8/fulltext
- https://www.jhsph.edu/covid-19/articles/side-effects-and-covid-19-vaccines-what-to-expect.html
- https://www.kff.org/coronavirus-covid-19/issue-brief/at-this-early-stage-of-the-covid-19-vaccine-roll-out-most-older-adults-have-not-yet-been-vaccinated-as-supply-remains-limited/
- https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html
- https://www.fda.gov/news-event…
- https://www.cdc.gov/mmwr/volumes/71/wr/mm7103a4.htm
Become a patient
Experience the Oak Street Health difference, and see what it’s like to be treated by a care team who are experts at caring for older adults.



