What Is Medicare Part C? Understanding Medicare Advantage
Article at a glance
Medicare Advantage (Part C) bundle Medicare Parts A and B of Original Medicare.
There are multiple types of Medicare Part C Plans to suit different income levels, health care needs, and treatment options.
Medicare Advantage Plans come with additional benefits not included within Original Medicare benefits, such as routine dental care, vision services, hearing services, wellness programs, and more.

Plenty of people may be familiar with the term “Medicare”—especially once they approach the age of 65. While Original Medicare is usually what comes to mind, there are other options that people can select from, such as plans called Medicare Advantage.
What Is the Federal Medicare Program?
The Federal Medicare Program is comprised of government-run health insurance plans for Americans age 65 and up, as well as younger Americans with disabilities and those with end-stage renal disease (ESRD).
There are two main ways to enroll in Medicare: Original Medicare or Medicare Advantage.
What Is Original Medicare?
Original Medicare is an option through the federal government that helps a person pay for health services as they need them. A patient can go to any doctor or hospital that accepts Medicare services to be treated, and Original Medicare will help to cover a significant portion of Medicare-approved costs. Original Medicare includes hospital insurance (Part A) and medical insurance (Part B).
Similar to Medicaid services, which focus on low-income patients, Medicare is a government-run program that can provide much-needed coverage for older patients’ health care needs.
What Is Medicare Part A?
Medicare Part A (hospital insurance) covers inpatient healthcare services such as:
Skilled nursing facility care
Nursing home care
Hospice care
Home health care
Medicare Part A normally comes premium-free for most beneficiaries if they have worked for at least 10 years and paid their Medicare taxes.
What Is Medicare Part B?
Medicare Part B (medical insurance) covers medically necessary outpatient healthcare and preventive services. Services covered include:
Clinical research
Ambulance services
Durable medical equipment (DME)
Limited outpatient prescription drug coverage
Medicare Part B also requires a monthly premium for most beneficiaries that is $164.90 in 2023.
What Isn’t Covered By Original Medicare?
Original Medicare covers a great deal of medical services, but there are some things it doesn’t automatically cover. Some examples of services and supplies not covered by Medicare include:
Dental
Vision
Hearing
Prescription drugs
Original Medicare beneficiaries can still get coverage for prescription drugs but would need to sign up for a Medicare drug plan in order to receive that coverage. These plans are known as Medicare Part D.
Note: Learn more about what isn’t covered by Original Medicare at this resource.
What Is Medicare Part D’s (Prescription Drug Coverage)?
Medicare Part D is Medicare’s prescription drug coverage. Medicare beneficiaries must either enroll in a separate Medicare drug plan to add on to their Original Medicare coverage or find a Medicare Advantage plan that includes drug coverage.
Note: Learn more about enrolling in Medicare Part D at this resource.
What Is Medicare Part C (Medicare Advantage)?
Medicare Advantage (also known as Part or MA plans) are Medicare health plans offered by private insurance companies. Medicare Advantage plans bundle Part A and Part B coverage into one health plan. That said, MA plans also include additional benefits such as coverage for dental, hearing, and vision services. Some Medicare Advantage plans also include prescription drug coverage.
Do note that not all Medicare Advantage plans provide coverage for prescription medications, so it’s important to check with the plan’s insurance company or a licensed insurance agent to see exactly what is included.
The difference with Medicare Advantage Plans versus Original Medicare is that Medicare Advantage plans often have their own network of healthcare providers and hospitals that a patient can use at a lower cost. A patient can opt to go outside of the provided network for medical services, but will likely pay more for those services.
Are There Different Types of Medicare Advantage Plans?
There are four main types of MA plans:
Health Maintenance Organizations (HMO)
Preferred Provider Organizations (PPO)
Private Fee For Services (PFFS)
Special Needs Plans (SNPs)
Each of these MA plans has different rules, costs, and coverage levels. Read on below to learn more about each type of MA plan.
Health Maintenance Organization (HMO)
HMO plans are based on a specific, agreed-upon network of doctors, providers, and hospitals within the plan. Patients are often required to choose their health care services and a primary care provider based upon that established network, with exceptions for emergency care or certain specialists that cover services not available within the HMO plan.
These plans tend to cost less than other options, so long as a beneficiary chooses within the network—if a beneficiary gets medical care outside of the network, the patient is then liable for the full medical cost.
Note: Learn more about HMO plans at this resource.
Preferred Provider Organization (PPO)
PPO plans allow for a patient to select from either an in-network line of healthcare providers and doctors or have the option to use any provider that accepts Medicare. Staying within the provided network will result in lower costs, whereas stepping outside the network will have a patient paying higher out-of-pocket costs.
That said, beneficiaries will still receive some coverage from their PPO plan if they go outside the network. This allows for much more flexibility on who can see, treat, and provide care.
Note: Learn more about PPO plans at this resource.
Private Fee For Service (PFFS)
PFFS plans decide beforehand how much a patient will have to pay for a healthcare provider, doctor, or hospital visit, and how much the plan will be willing to pay for those medical services. Some plans have a network of providers to choose from, while others do not. A patient can also choose to go outside the network, however, they must confirm with doctors, specialists, or providers that they will agree to treat them under the plan’s terms.
PFFS plans can provide some flexibility in terms of care, but also run the potential risk of not finding preferred providers who will work with the plan’s payment terms.
Note: Learn more about PFFS plans at this resource.
Special Needs Plans (SNP)
This type of plan is only available to people with specific diseases, and the plan tailors specifically to that particular group of people. Plans vary in terms of provided in-network and out-of-network options, so it’s important to check with each individual plan. Typically, SNPs do have specialists in the diseases and conditions that affect their patients.
Note: Learn more about SNP plans at this resource.

When To Enroll in Medicare Advantage
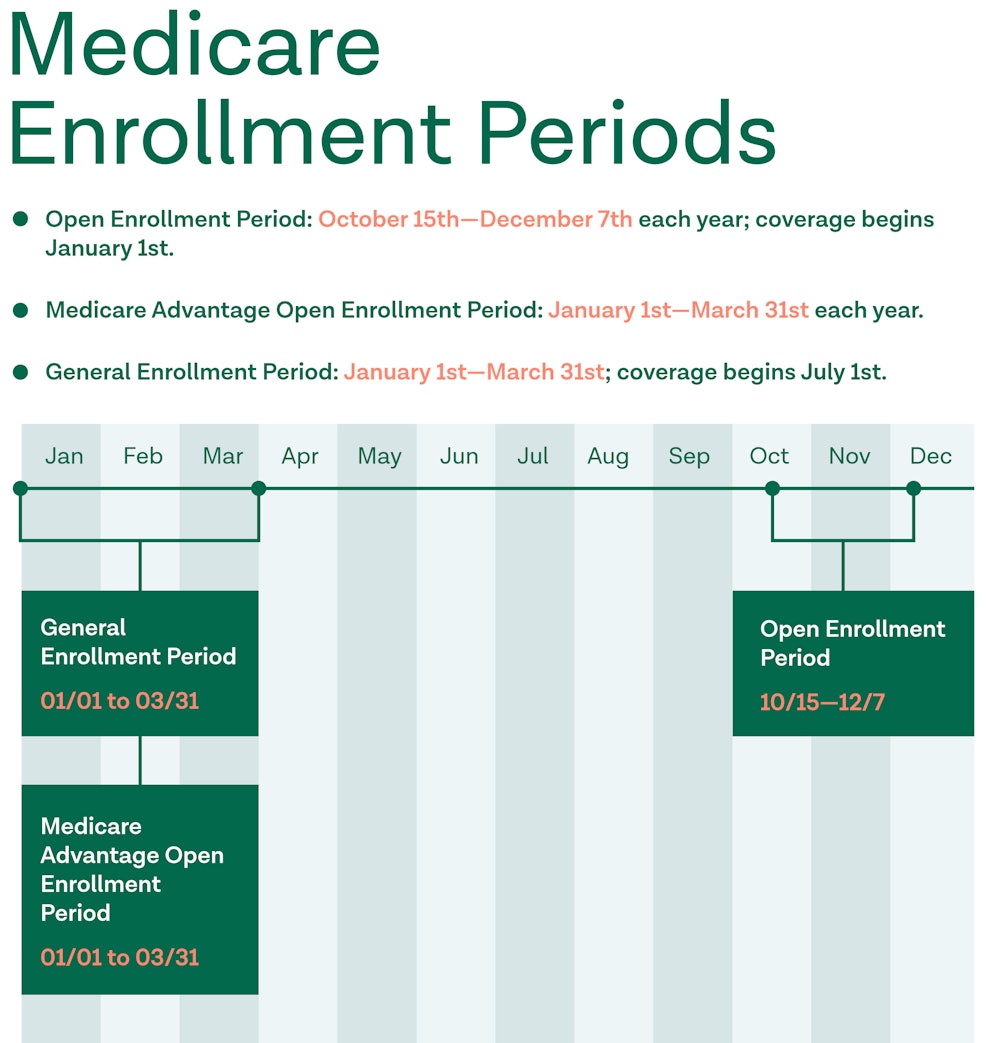
In order for a person to qualify for a Medicare Advantage Plan, they must qualify for Original Medicare. While in most cases a person is automatically enrolled in Medicare once they turn 65, there may be circumstances where they need to sign up for Original Medicare during a specific enrollment period. These periods include:
Initial Enrollment Period (IEP): Enrollment for Original Medicare begins three months before a person’s 65th birthday, and the window lasts for seven months.
General Enrollment Period (GEP): If a person didn’t sign up during the initial enrollment period, they can sign up during the general enrollment period, which goes from January 1st through March 31st. General enrollment for most Medicare Advantage Plans falls between April and June (check with each specific plan for dates).
Special Enrollment Period (SEP): If a person is unable to sign up for Medicare during the initial and general enrollment periods due to specific circumstances, they may qualify for a Special Enrollment Period. The dates vary for the period based on the surrounding events and circumstances that qualified them.
However, in order to switch to a Medicare Advantage Plan, a person must enroll during a different period to do so. This is known as the Fall Enrollment Period (FEP), which runs from October 15-December 7th of each year.
How To Enroll in Medicare Advantage
Once someone is able to enroll in Medicare, they need to take the time to compare different Medicare Advantage Plans in their area. They can do so using the Medicare federal government website’s Medicare Plan Finder tool.
Once they’ve settled on a potential plan, a beneficiary can do the following:
Visit the Medicare Advantage Plan’s website to see if there is an option to join online.
Contact the plan to get a paper enrollment form, fill it out, and return it to the plan. All plans must offer this option.
Call the plan directly by getting their contact information
Call the Medicare.gov phone number at 1–800-MEDICARE.
Other Supplemental Medicare Plans
What Is Medigap?
Medicare Supplement Insurance—also known as Medigap—helps cover insurance costs that Original Medicare doesn’t cover. Unlike the federal Medicare program, Medigap is offered by private health insurance companies.
After Medicare covers its agreed-upon costs, Medigap serves as additional coverage. Medigap helps to pay a Medicare-approved amount of leftover costs—including copayments, coinsurance, and deductibles. Additionally, Medigap can offer options that Original Medicare doesn’t, like medical services when you travel outside of the U.S.
To learn more about Medigap coverage, visit this source.
What Is Dual Eligibles?
Dual Eligibles are people who qualify for both Medicaid and Medicare. Due to this, they have the ability to combine them into one program where Medicare is the primary insurance and Medicaid is the supplementary insurance. Medicaid services and programs are often targeted at the state level, and most health expenses are taken care of for someone who qualifies for dual eligibility.
To learn more about enrollment for Dual Eligibles, visit this source.
Sources
https://www.medicare.gov/what-medicare-covers/your-medicare-coverage-choices/whats-medicare
https://www.medicare.gov/Pubs/pdf/11306-Medicare-Medicaid.pdf
https://www.medicare.gov/what-medicare-covers/what-part-a-covers
https://www.medicare.gov/what-medicare-covers/what-part-b-covers
https://www.medicare.gov/what-medicare-covers/whats-not-covered-by-part-a-part‑b
https://www.medicare.gov/sign-up-change-plans/types-of-medicare-health-plans/special-needs-plans-snp
Medicare Part C Breakdown
This infographic explains the basics of Medicare Part C or Medicare Advantage.




