
How to Check Medicare Application Status
There are a few different ways one can check the status of their Medicare application, such as:
Logging into one’s “My Social Security” account via the Social Security website.
Visiting a local Social Security office. To find a Social Security office in one’s community, visit this source.
Contact Social Security Administration by calling 1–800-772‑1213 (TTY 1–800-325‑0778) anytime Monday through Friday, 7 a.m. to 7 p.m.
Visiting the “Check Enrollment” section of one’s “My Medicare” account. Visiting the online Medicare account may save an enrollee time via visiting an in-person location or calling a center.
Note: Checking the application status via one’s Social Security (SSA) account will require an enrollee to enter their Social Security number and their application confirmation number. However, it’s important to note that the SSA website is secure and an enrollee’s private information will not be shared or stored.

What the SSA Application Status Will Show
Once the enrollee logs into their SSA account, their application status will show:
The date when the application was filed.
Where the claim is currently located and the office that is servicing that claim.
A scheduled hearing date and time for the specific claim.
Numbers for re-entry if there are incomplete portions of the application.
Various publications that may be of interest depending on the claim and where it’s at in its processing.
Note: Once an application/claim has been processed, the enrollee will receive a letter in the mail notifying them on the result. If the enrollee has been rejected, specifications will be listed as to why they were turned away.
How to Check Medicare Advantage Plan Status
Medicare Advantage plans, sometimes called Medicare Part C, are Medicare supplemental insurance plans for they work to fill the gaps in standard Medicare coverage. Medicare Advantage plans are processed differently than standard Medicare as they are administered by private health insurance companies that hold contracts with the federal Medicare program. Therefore, in order for an enrollee to check their MA plan status, they must reach out to the private health insurance company that they applied through.
How to Check Medicare Part D (Prescription Drug) Status
Medicare Part D is known as the prescription drug coverage for standard Medicare plans. Similar to MA plans, Medicare Part D is administered via private health insurance companies that have contracts with the federal Medicare program. In order for an enrollee to check their Medicare Part D application status, they must contact the member services department of the health insurance provider they applied through. Another common way enrollees check their Part D status is by having their pharmacy file a test claim.

How to Check Medigap (MedSupp) Application Status
Medigap plans, otherwise known as MedSupp, are considered to be supplemental Medicare plans and therefore are applied for differently than Original Medicare. Medigap plans are administered through private health insurance companies that have contracts with the federal Medciare program. Therefore, in order to check one’s Medigap application status, one should contact the insurance company they applied through or reach out to 1–800-MEDIGAP (1–800-633‑4427).
What Comes After the Application Process
After the application has been processed, the enrollee will receive a letter in the mail specifying their acceptance or rejection from the federal Medicare program.
What an Approved Enrollee Receives
If an individual is notified that they have been approved for Medicare, then they should soon receive a “Welcome to Medicare” package in the mail. This welcome package includes a guidebook that leads them through the various Medicare benefits and options made available to them through their plan. The package will also include the enrollee’s Medicare insurance card.
Note: To read the “Welcome to Medicare” package for those automatically enrolled, visit this source. To read the “Welcome to Medicare” package for those who applied, visit this source.
Overview of a Medicare Card
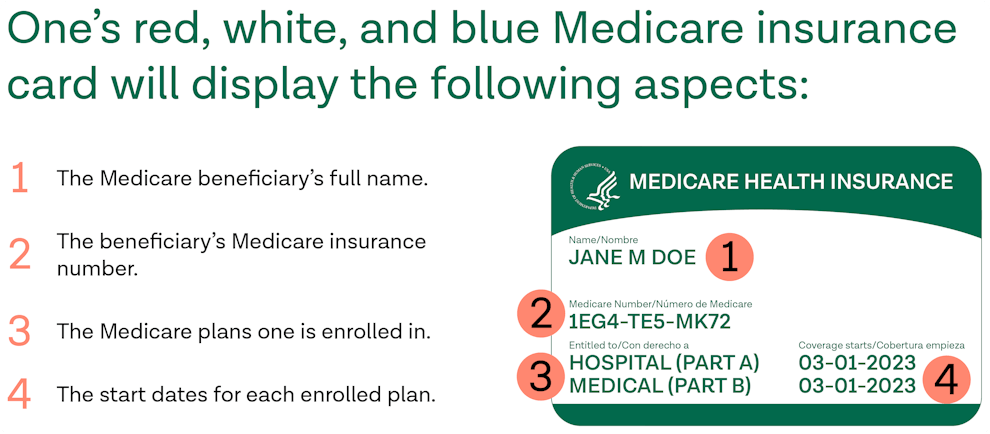
One’s red, white, and blue Medicare insurance card will display the following aspects:
The Medicare beneficiaries full name.
The beneficiaries Medicare insurance number.
The Medicare plans one is enrolled in.
The start dates for each enrolled plan.
Separate insurance cards will be mailed to individuals enrolled in Medicare Advantage (MA) plans or Medicare Part D plans.
Note: To learn more about the Medicare insurance card and see a sample of what one looks like, visit this source.
What Happens When an Application is Not Accepted
When an individual is denied from the federal Medicare program, they will receive a letter from the SSA explaining why they haven’t been approved and the steps to take moving forward.

Date When Coverage Begins for Beneficiaries
Coverage begins for patients depends on a variety of factors including if a patient is eligible for automatic enrollment or must apply for enrollment.
Note: To learn more about Medicare eligibility and who can enroll, visit this source.
Automatic Enrollment Coverage
Patients eligible for automatic enrollment in Medicare Part A (hospital insurance), have the option to enroll through a seven month period called “initial enrollment period” (IEP). The initial enrollment period spans from the three months prior to the individual’s birth month, the individual’s birth month, and three months after the individual’s birth month. Coverage for these beneficiaries depends on the month they choose to register:
Sign Up Before One Turns 65: Coverage begins the month one turns 65.
Sign Up During Their Birth Month: Coverage begins at the beginning of the following month.
Sign Up One Month After They Turn 65: Coverage begins on the first of the month two months after the sign up month.
Sign Up During Last Two Months of IEP: Coverage begins on the first of the month three months after the sign up month.
Application Enrollment Coverage
If one enrolls in Part A via an application process, their coverage begins six months after their sign up month. Coverage cannot begin earlier than the month one turns 65.
Note: To learn more about coverage timeframes, visit this source.
Note: Medicare Part B (medical insurance) must be applied for separately. To learn more about the parts of Medicare and how to apply, visit this source.
Other Medicare Enrollment Periods
Medicare offers a wide range of enrollment periods including the initial enrollment period (IEP), open enrollment period (OEP), special needs periods (SNP), general enrollment period (GEP), and more.
Sources
Become a patient
Experience the Oak Street Health difference, and see what it’s like to be treated by a care team who are experts at caring for older adults.



