Article at a glance
In most cases, Medicare only covers emergency transportation. However, there are situations where there will be Medicare transportation coverage for non-emergency, medically necessary services, such as in treatments for ESRD. A doctor’s note will be necessary.
Some Medicare Advantage plans may have transportation as an added benefit, but this will vary greatly per plan. Medicare beneficiaries should always confirm with their insurance plan.
Medicaid provides a non-emergency transportation service for eligible members known as Non-Emergency Medical Transportation (NEMT). How the service functions will depend on the beneficiary’s location.
Medigap helps cover costs associated with ambulance services, but not ambulance services themselves.
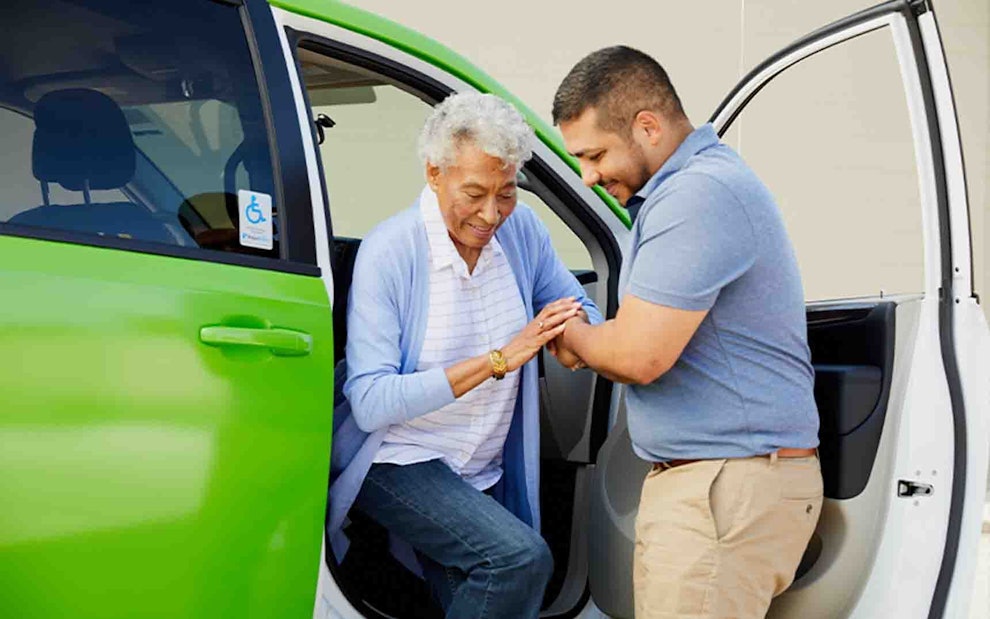
There are other options for transit to medical appointments, including Uber Health, Lyft Pass for Healthcare, and Oak Street Health’s green van service.
As Americans grow older, their access to transportation may become diminished. Understandably, this can be an upsetting experience and a cause for concern. After all, transportation affects every part of modern life, including being able to see family and friends, purchase groceries, and run other important errands.
Reliable transportation is also vital when it comes to getting to and from medical appointments. Medicare beneficiaries with limited access to transportation will be relieved to know there are services in place for senior citizens to receive medical care, no car or driver’s license necessary. This article will explain how medical transportation services work with Medicare coverage, government programs, and more.
Does Medicare Cover Transportation Services?

Original Medicare does not cover any non-emergency transportation services, such as traveling to routine health care appointments. However, Original Medicare covers emergency ambulance transportation services.
Emergency Transportation and Medicare Coverage
Medicare Part B covers emergency transportation services for those who need to go to a hospital, critical access hospital, or a skilled nursing facility to receive emergency services. However, the following criteria must be met in order for Medicare Part B to cover an ambulance ride:
The services needed are for medical emergencies (i.e. a heart attack or stroke)
Ground ambulance transport is safe, meaning traveling in other vehicles would be more dangerous for the patient
In dire medical situations where ground transportation via ambulance is not fast enough to get patients the care they need, Medicare Part B may also provide coverage for emergency transportation via airplane or helicopter.
Note: Learn more about Medicare plans work with ambulance transportation at this resource.
Original Medicare Transportation Costs
For emergency ambulance transportation, Medicare beneficiaries pay 20 percent of the Medicare-Approved amount. The Medicare Part B deductible will also apply. In 2021, Medicare Part B’s deductible is $203.
Non-Emergency Ambulance Transportation
Original Medicare does not cover non-emergency transit, such as getting to and from doctor’s appointments. However, there are situations in which Medicare Part B may cover non-emergency ambulance services. An example of this would be for someone with End-Stage Renal Disease (ESRD) needing medically necessary ambulance transport to a medical facility that provides dialysis.
In order for non-emergency transportation to be covered, beneficiaries will need a note from their doctor confirming that ambulance transportation for the given situation is medically necessary. As well, Medicare Part B only covers non-emergency transit to the nearest appropriate medical facility. If a medical facility is farther away,
From there, a few things may occur. The ambulance company might potentially give the patient an Advance Beneficiary Notice of Noncoverage (ABN). For reference, an ABN is a form that is provided by a health care provider to Medicare beneficiaries when they anticipate Medicare won’t provide coverage for a particular healthcare service. This is done to transfer financial liability to the beneficiary.
In the event someone receives an ABN, they have two options: they can decline the service or agree to the ABN. Once someone agrees to an ABN, however, they are responsible for all the costs if it is not covered under Medicare Part B.
Do Medicare Advantage Plans Cover Transportation Services?
Medicare Advantage (MA) plans, or Medicare Part C, have, at minimum, the same covered services as Original Medicare. In addition, Medicare Advantage plans are unique in that these health plans provide additional benefits that Original Medicare does not.
Some benefits a Medicare Advantage plan may include are additional coverage for prescription drugs, hearing, dental, and vision. Transportation benefits may also be included.
Beneficiaries should consult their insurance plan to confirm or speak with a licensed insurance agent. Oak Street Health has trained professionals that are able to guide patients through their health insurance benefits if needed.
Does Medicaid Cover Transportation Services?
Medicaid is a state and federal program that works together to provide healthcare for those with lower levels of income. Medicaid covers emergency trips in ambulances.
Medicaid may also cover non-emergency transportation to health appointments at a doctor’s office or clinic. This is known as Non-Emergency Medical Transportation (NEMT).
What to Know About NEMT
Those eligible for NEMT have to meet certain criteria. Some situations that may merit coverage include:
No driver’s license
No car (or a car that doesn’t work)
Physical or mental disability
Inability to travel or wait for rides alone
Rules for this service will vary by state. For example, those who schedule non-emergency, medically necessary transportation through an ambulance company based in New Jersey, Pennsylvania, or South Carolina may need to obtain prior authorization. As such, any beneficiary interested in this service should contact their State Medicaid Agency for approval and more information.
Note: Medicare beneficiaries can enroll in Medicaid and still keep their Medicare coverage. This is known as the Dual-Eligibles program.

Do Medigap (MedSupp) Plans Cover Transportation Services?
Medicare supplement insurance plans, known as Medigap or MedSupp, “fill in the gaps” of Original Medicare coverage. One way these supplemental plans fill in the coverage gap is by assisting with deductible, copayment, and coinsurance payments.
When it comes to ambulance transport, Medigap plans do not directly cover this service. That said, Medicare supplement plans generally do help cover the Medicare Part B annual deductible. MedSupp plans may also cover coinsurance payments.
As mentioned previously, Part B’s deductible applies for ambulance rides, as does a 20% Medicare-approved Amount for the service. This is when a Medigap plan may step in and cover the deductible and coinsurance payment.
Non-Medicare Transportation Options

In the event a Medicare beneficiary requires transportation but does not have transportation coverage through their insurance, there are other ways to ensure their transportation needs are met.
RideShare Apps
In April 2021, the ride-sharing app Lyft announced Lyft Pass for Healthcare. This new product was created for eligible patients, including those with Medicare and Medicaid, to order Lyft rides specifically for health appointments through the Lyft app.
According to the official Lyft press release, “The sponsoring healthcare or social services organization still covers the cost of the ride, while having access to built-in controls for budget, location, compliance, and more.”
Those interested in Lyft Pass For Healthcare should confirm this benefit with their Medicare plan.
Uber Health is another option. Uber Health helps senior citizens book trips to their medical appointments without requiring the patient to have to sign up for the Uber app. Learn more here.
Programs of All-Inclusive Care for the Elderly (PACE)
Programs of All-Inclusive Care for the Elderly, or PACE, is a jointly-run program by Medicare and Medicaid. PACE benefits include services covered by Medicare and Medicaid, in addition to other services, including transportation. Those eligible for PACE will also have an interdisciplinary team to coordinate their medical care. This includes a driver.
Note: Learn more about the voluntary PACE program at this resource.
Area Agencies on Aging (AAA)
Area Agencies on Aging, or AAA, are local organizations that may provide transportation services. Visit this resource to learn more about AAA and find a local AAA branch.
FAQ
Does Medicare cover ambulance services?
In short, it depends on the circumstances. Medicare covers ground ambulance transportation and at times, emergency air transport when patients are in dire circumstances. Medicare Part B will also cover transport if healthcare providers deem it medically necessary for an ambulance to take patients with particular conditions (such as ESRD) to the nearest hospital or treatment facility.
Can I use Medicare while out of state?
Yes, your Medicare insurance will be accepted at any practice that accepts Medicare within the United States.
Should I carry my Medicare card when I travel?
Absolutely. Your Medicare insurance card is valid at any practice that accepts Medicare in the United States.
What should I do if Medicare denies my ambulance service even though it should be covered?
It’s possible that the ambulance company did not properly file the paperwork or did not accurately fill out why the ambulance was necessary. You can find the ambulance company’s information on your Medicare Services Notice (MSN) and file a claim or an appeal to receive coverage. For more information on appealing denied coverage for ambulance transportation, visit this resource.
Become a patient
Experience the Oak Street Health difference, and see what it’s like to be treated by a care team who are experts at caring for older adults.



